For children with Cerebral Palsy (CP), the intricate coordination of the mouth, tongue, jaw, and palate – collectively known as oral motor skills – forms the bedrock of two fundamental aspects of life: feeding and speech. When these skills are challenged due to neurological impairments, the impact can extend far beyond mere mechanics, affecting nutrition, communication efficacy, social engagement, and ultimately, the child’s overall well-being. Effectively managing oral motor skills through targeted interventions and a collaborative approach is paramount to fostering safer and more efficient feeding, as well as clearer and more understandable speech. This comprehensive guide delves into the multifaceted challenges of oral motor dysfunction in CP and explores a range of practical strategies and therapeutic approaches designed to empower these children.
Unraveling the Complexities of Oral Motor Challenges in CP
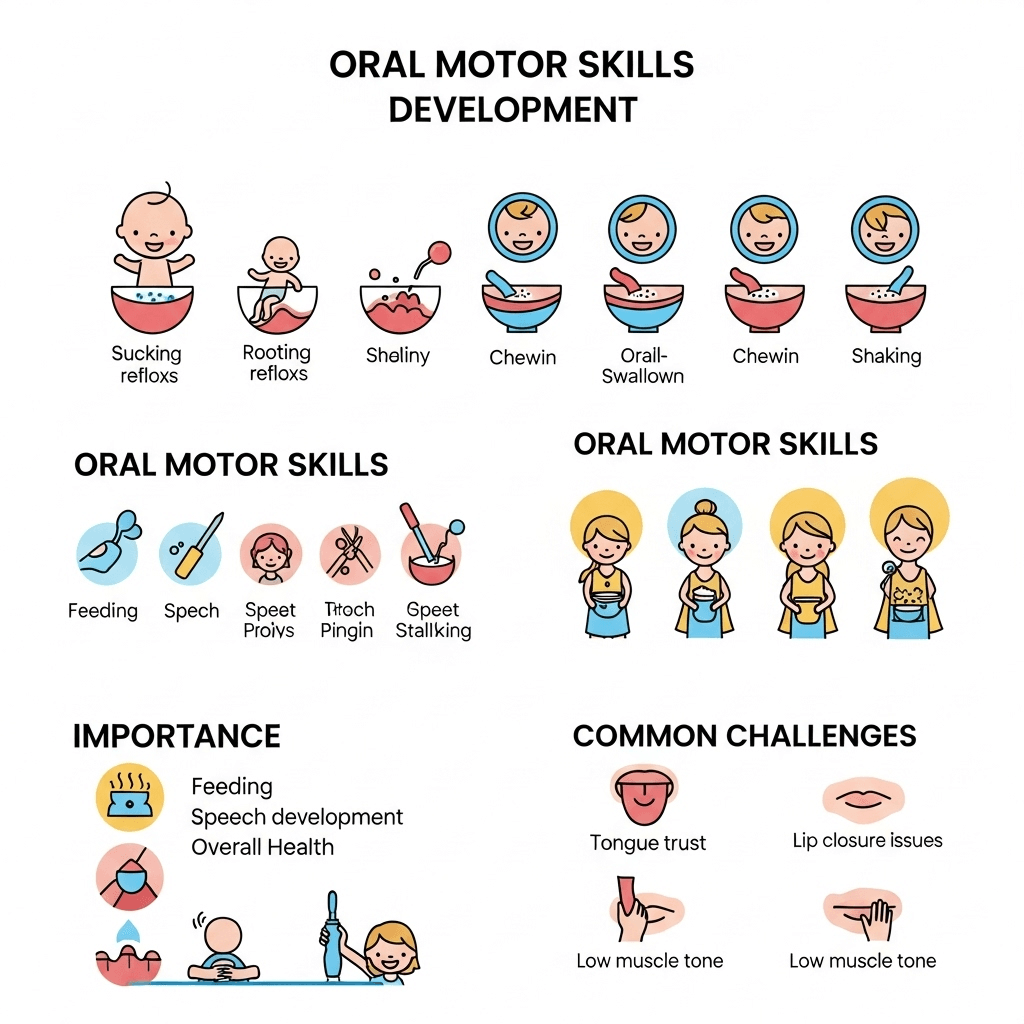
The diverse nature of brain involvement in CP manifests in a spectrum of oral motor difficulties. Understanding these specific challenges is the first step towards effective management:
- Dysphagia: The Silent Threat: Swallowing, a seemingly automatic process, becomes a significant concern when oral motor coordination is impaired. Dysphagia in children with CP can range from mild difficulties with certain textures to severe impairments leading to aspiration – the dangerous entry of food or liquid into the airway. This not only poses an immediate health risk but can also lead to recurrent respiratory infections and impact nutritional intake.
- The Unsealed Lips: Impact of Poor Labial Closure: The simple act of closing the lips plays a crucial role in containing food and saliva within the mouth, as well as forming essential speech sounds like /p/, /b/, and /m/. Children with weak lip closure may experience persistent drooling, messy eating habits that can affect social acceptance, and difficulty articulating these key phonemes, impacting speech intelligibility.
- Tongue Thrust: A Persistent Pattern: An abnormal, forceful protrusion of the tongue, often beyond the lips, is a common oral motor pattern in some children with CP. This tongue thrust can interfere with the normal mechanics of swallowing, pushing food out of the mouth. Over time, it can also affect the development of a mature swallow pattern, impact articulation, and even contribute to dental malocclusion.
- The Mobile Maestro: Limitations in Tongue Movement and Coordination: The tongue is a highly agile muscle crucial for manipulating food within the mouth for chewing, forming a bolus for swallowing, and articulating a vast array of speech sounds. Restricted range of motion, weakness, or discoordination of the tongue can severely impact both feeding efficiency and speech clarity. Difficulty moving the tongue laterally, elevating its tip, or retracting it can hinder chewing, bolus formation, and the production of sounds like /l/, /r/, /s/, and /z/.
- The Unstable Foundation: Jaw Instability or Weakness: The jaw provides the stable base upon which the lips and tongue operate. Poor jaw control, characterized by excessive opening, instability during chewing, or weakness, can make it difficult to bite, chew effectively, and produce clear speech sounds that require controlled jaw movements.
- The Inefficient Processor: Weak or Uncoordinated Chewing: Effective chewing is essential for breaking down food into manageable pieces for safe swallowing and for stimulating saliva production, which aids digestion. Children with CP may exhibit weak or uncoordinated chewing patterns, leading to prolonged mealtimes, fatigue during eating, and an increased risk of choking on larger food particles.
- The Garbled Message: Articulation Difficulties (Dysarthria): Dysarthria, a motor speech disorder, is common in CP and results from weakness, slowness, or incoordination of the muscles used for speech production, including the lips, tongue, jaw, and vocal cords. This can lead to slurred, imprecise speech that is difficult for others to understand, impacting social interaction and academic participation.
- The Unaware Navigator: Reduced Oral Sensation: Decreased sensitivity within the mouth can impair a child’s awareness of food or saliva, making it harder to control these substances effectively and increasing the risk of aspiration or food remaining in the mouth after swallowing.
A Symphony of Strategies: Therapeutic Interventions for Oral Motor Skills
Addressing the multifaceted oral motor challenges in CP necessitates a collaborative effort from a dedicated multidisciplinary team. Speech-language pathologists (SLPs) often take the lead in oral motor therapy, working closely with occupational therapists (OTs), feeding specialists, dietitians, and the child’s family to develop and implement individualized intervention plans:
Feeding Therapy: Cultivating Safe and Enjoyable Mealtimes
- The Importance of Posture: Optimal Positioning for Safe Swallowing: Proper positioning during feeding is foundational for maximizing oral motor control and ensuring a safe swallow. This often involves utilizing specialized seating systems that provide adequate trunk support, head alignment, and pelvic stability. Occupational or physical therapists play a crucial role in determining the most appropriate positioning to minimize the risk of aspiration and facilitate efficient oral motor movements.
- Creating a Calm Culinary Space: Environmental Modifications for Focused Eating: A chaotic or distracting feeding environment can exacerbate oral motor difficulties. Minimizing visual and auditory distractions can help the child focus on the task of eating, improving their ability to control oral movements and swallow safely.
- Tailoring Textures: The Art of Food Modification: Adapting the consistency of food to match the child’s current oral motor and swallowing abilities is paramount. This may involve progressing through a continuum of textures, from smooth purees to soft solids and eventually to chopped or table foods, as the child’s skills improve. Careful assessment by the feeding team guides these modifications to ensure both safety and adequate nutritional intake.
- Tools for Success: Adaptive Equipment for Enhanced Feeding: Specialized spoons with shallow bowls, angled handles, or non-slip grips, as well as adapted cups with spouts or controlled flow, can significantly enhance a child’s ability to self-feed safely and efficiently, promoting independence and reducing frustration.
- Exercising the Oral Muscles: Targeted Drills for Feeding Proficiency: Specific oral motor exercises, often playful and engaging, are designed to improve the strength, range of motion, and coordination of the lips, tongue, and jaw for feeding. These might include lip closure exercises using straws or spoons, tongue lateralization activities with food placed on the sides of the mouth, and jaw stability exercises involving controlled biting and chewing on textured objects.
- Mastering the Swallow: Teaching Safe and Effective Techniques: Children with dysphagia may benefit from learning specific swallowing strategies, such as the chin tuck maneuver to protect the airway, or the use of multiple swallows to clear any remaining food in the pharynx. The feeding therapist carefully assesses the child’s swallow mechanism and teaches compensatory strategies as needed.
- Navigating Sensory Worlds: Addressing Food Sensitivities: Many children with CP also experience sensory processing differences that can impact their acceptance of various food textures and tastes. A gradual and systematic approach to introducing new sensory experiences with food, often involving play-based exploration, can help to reduce food aversions and expand dietary variety.
Speech Therapy: Finding and Amplifying the Voice
- Oral Gymnastics for Speech: Targeted Exercises for Articulation Clarity: Similar to feeding exercises, specific oral motor exercises are crucial for improving the strength and coordination of the articulators (lips, tongue, jaw) for speech production. These might involve repetitive movements like lip rounding and spreading, tongue tip elevation and lateralization, and controlled jaw opening and closing, often presented in a fun and motivating way.
- The Art of Sound Production: Articulation Therapy with Multi-Sensory Cues: Speech-language pathologists utilize a variety of techniques to teach the correct production of individual speech sounds that are challenging due to oral motor impairments. This often involves visual cues (e.g., showing the child how to position their mouth), auditory cues (e.g., emphasizing the target sound), and tactile cues (e.g., physically guiding the child’s articulators).
- Bridging the Communication Gap: Augmentative and Alternative Communication (AAC) as a Supportive Tool: When verbal speech is significantly limited, exploring and implementing appropriate Augmentative and Alternative Communication (AAC) methods becomes essential for providing the child with a reliable means of expression. This can range from low-tech options like picture communication boards to high-tech speech-generating devices, ensuring that the child has a “voice” regardless of their oral motor abilities.
- The Melody of Speech: Training Prosody and Intonation: Oral motor control also influences the rhythm, stress, and intonation of speech, which are crucial for conveying meaning and emotion. Therapy may target improving breath control and the smooth flow of speech to enhance prosodic elements.
- The Power of Breath: Exercises for Sustained Speech: Adequate breath support is fundamental for producing sufficient volume and sustaining speech sounds. Exercises that focus on improving breath control and coordination with oral movements can lead to clearer and more audible speech.
Synergistic Approaches: Integrating Care for Holistic Progress
- The Intertwined Skills: Recognizing the Overlap Between Feeding and Speech: Therapists recognize that many of the underlying oral motor skills required for safe and efficient feeding are also essential for clear articulation. Intervention plans often incorporate exercises and strategies that benefit both areas, maximizing efficiency and progress.
- Addressing the Sensory Foundation: Sensory Integration for Improved Oral Motor Control: For children whose oral motor difficulties are intertwined with sensory processing challenges, incorporating sensory integration techniques can be beneficial. Addressing sensitivities or seeking behaviors related to oral input can create a more receptive environment for oral motor skill development.
- Harnessing Technology: Neuromuscular Electrical Stimulation (NMES) as an Adjunct: In select cases of significant oral muscle weakness, Neuromuscular Electrical Stimulation (NMES) may be considered as an adjunct therapy. This technique uses mild electrical currents to stimulate muscle contraction, potentially improving strength and function.
Empowering Caregivers: Practical Tips for Home Support
The consistency and support provided at home play a vital role in reinforcing the progress made during therapy sessions:
- A United Front: Working in Tandem with the Therapy Team: Open communication and collaboration with the child’s therapists are crucial. Actively follow their recommendations and consistently practice assigned exercises at home.
- The Power of Repetition: Patience and Consistency in Practice: Developing oral motor skills takes time and consistent effort. Be patient with your child and provide regular opportunities for practice in a supportive and encouraging manner.
- Creating Positive Associations: Fostering Enjoyable Mealtime Experiences: Avoid creating pressure or anxiety around mealtimes. Focus on making eating a positive and social experience.
- The Keen Observer: Documenting Progress and Challenges: Pay close attention to your child’s oral motor skills during feeding and speech attempts. Document any changes or ongoing difficulties and share these observations with the therapy team to inform treatment adjustments.
- Adapting to Needs: Modifying the Environment and Utilizing Tools: Implement recommended food texture modifications and consistently use any adaptive equipment provided by the therapists.
- Communication is Key: Encouraging Expression in All Forms: Support your child’s attempts to communicate in any way they can, whether through verbalizations, gestures, signs, or their AAC device. Every attempt to communicate is a step forward.
- Finding Strength in Numbers: Connecting with Support Groups: Connecting with other families who understand the challenges of managing oral motor skills in CP can provide invaluable emotional support, practical tips, and a sense of community.
For a wealth of additional information and supportive resources related to feeding and communication strategies for children with Cerebral Palsy, we encourage you to explore the dedicated sections on CP Family Hope: Daily Living and Communication and Language.
Looking Ahead: Building Stronger Foundations for Nourishment and Connection
Managing oral motor skills in children with Cerebral Palsy is a journey that requires patience, expertise, and a collaborative spirit. By embracing comprehensive assessment, implementing targeted and evidence-based therapies, and providing consistent support within the home environment, we can empower these children to develop stronger foundations for safe and efficient feeding, as well as clearer and more meaningful communication, ultimately enriching their lives and fostering greater independence.
Frequently Asked Questions: Navigating Oral Motor Skill Management in CP
Why are oral motor skills so frequently affected in children diagnosed with Cerebral Palsy?
The primary reason lies in the nature of CP itself – a neurological disorder resulting from brain damage that occurs before, during, or shortly after birth. This brain injury can disrupt the neural pathways that control the complex coordination of the muscles in the face, mouth, tongue, and jaw, leading to a range of challenges including weakness, incoordination, and abnormal muscle tone.
What specific role does a speech-language pathologist play in addressing oral motor skill deficits?
Speech-language pathologists (SLPs) are the primary professionals trained to assess and treat oral motor difficulties that impact both feeding and speech. Through comprehensive evaluations, they identify specific areas of weakness or discoordination and develop individualized therapy plans that incorporate targeted exercises, compensatory strategies, and adaptive techniques to improve function and safety.
As a caregiver, what are some practical ways I can reinforce oral motor skill development at home?
Consistency is key. Work closely with your child’s therapists to understand the recommended exercises and integrate them into your daily routines in an engaging and playful manner. Be patient, provide positive reinforcement for effort, and create a supportive environment that encourages practice without pressure.
Is it realistic to expect significant improvements in feeding and speech for a child with severe oral motor challenges?
While the degree of progress varies depending on the severity of the initial impairment and the child’s individual response to therapy, many children with significant oral motor challenges can achieve meaningful improvements in both feeding safety and efficiency, as well as speech clarity, through consistent and appropriate intervention. Augmentative and Alternative Communication (AAC) can also play a vital role in ensuring effective communication, even if verbal speech remains limited.
At what stage of development should oral motor therapy typically commence for a child with a CP diagnosis?
Early intervention is paramount. If feeding difficulties or early signs of communication delays are identified in infancy, oral motor therapy can and should begin as early as possible. The brain’s greater plasticity in the early years allows for more significant impact from therapeutic interventions.
👉 Fill out our FREE Consultation Form today to speak with a legal expert. Your case could make a difference.