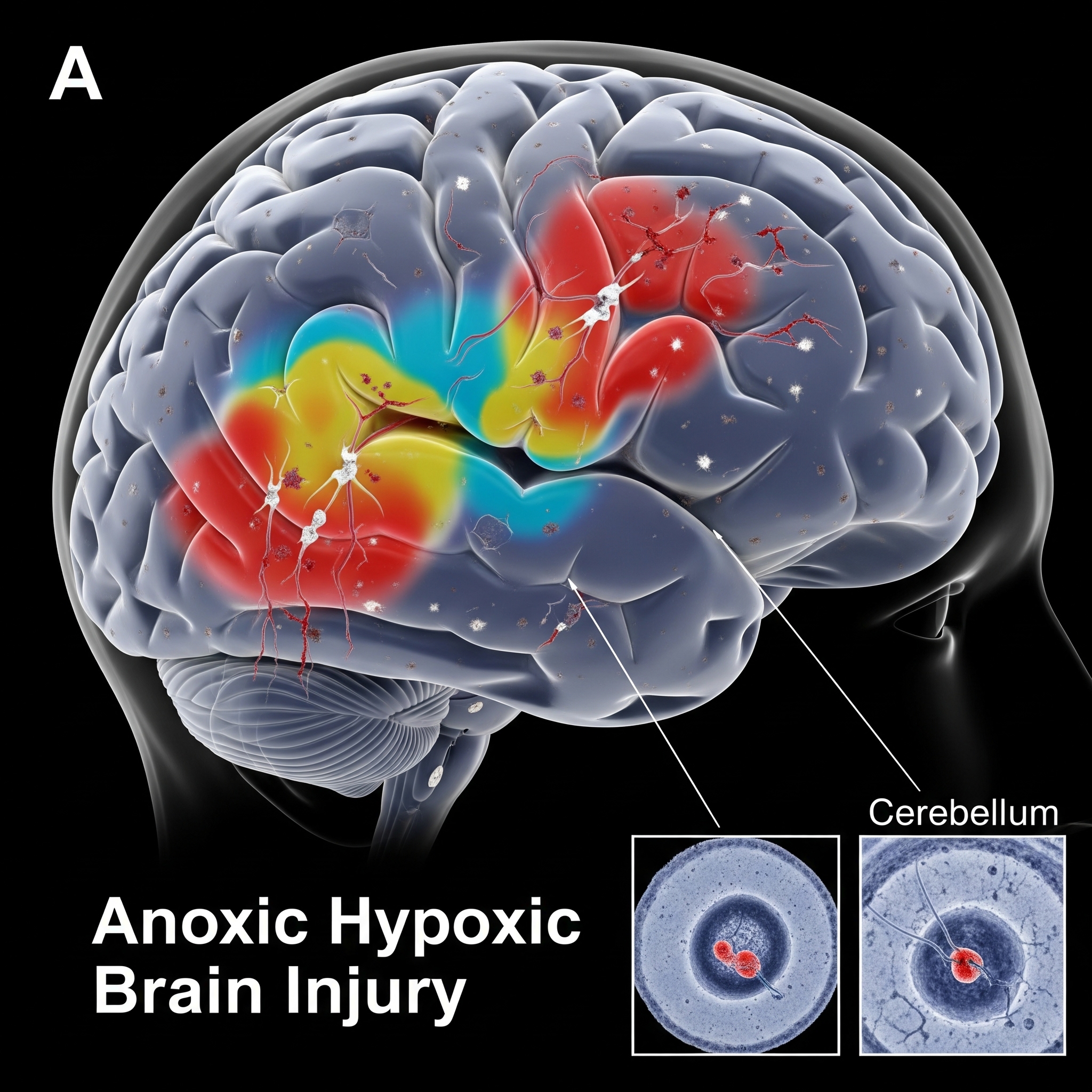
When a newborn’s brain is deprived of oxygen during birth, the consequences can be devastating, often leading to severe and lifelong neurological impairments. These injuries are broadly categorized as either anoxic or hypoxic. Understanding the precise differences between Anoxic Hypoxic Brain Injury is crucial for families, as these distinctions can influence diagnosis, prognosis, and the legal strategies employed in a birth injury claim. This article delves into the nuances of Anoxic Hypoxic Brain Injury, clarifying these critical medical terms.
Understanding Anoxic Hypoxic Brain Injury: The Core Difference
Both anoxia and hypoxia refer to conditions involving oxygen deprivation to the brain. The key distinction in Anoxic Hypoxic Brain Injury lies in the degree of oxygen deficiency:
1. Anoxic Brain Injury
- Definition: Anoxic brain injury occurs when there is a complete absence of oxygen supply to the brain. This is the more severe form of oxygen deprivation.
- Causes: Typically results from events that completely cut off blood flow to the brain, such as severe umbilical cord compression, prolonged cardiac arrest, or profound shock.
- Impact: Due to the complete lack of oxygen, anoxic brain injuries often lead to very severe and widespread brain damage, with potentially more profound neurological deficits.
2. Hypoxic Brain Injury
- Definition: Hypoxic brain injury occurs when there is a partial, but significant, reduction in oxygen supply to the brain.
- Causes: Can result from conditions that reduce oxygen in the blood (e.g., severe maternal anemia, respiratory distress) or conditions that reduce blood flow to the brain (e.g., sustained low maternal blood pressure). Hypoxic-Ischemic Encephalopathy (HIE) is a specific type of hypoxic-ischemic injury.
- Impact: The severity of damage varies depending on the degree and duration of oxygen deprivation. While still very serious, the impact can sometimes be less widespread than anoxic injuries, though still leading to significant impairments like cerebral palsy.
The distinction between Anoxic Hypoxic Brain Injury is vital because it helps medical professionals pinpoint the precise cause of the damage and predict the likely outcomes.
Causes of Anoxic Hypoxic Brain Injury at Birth
Both types of Anoxic Hypoxic Brain Injury at birth can be caused by preventable medical errors. Common factors include:
- Umbilical Cord Complications: Prolapsed cord, nuchal cord (cord around the neck), or true knots can severely restrict or cut off oxygen.
- Placental Issues: Conditions like placental abruption (placenta detaching from the uterus) or placenta previa can lead to severe oxygen deprivation.
- Maternal Health Crises: Severe maternal hypotension, hemorrhage, or cardiac arrest.
- Prolonged or Obstructed Labor: If the labor is excessively long or if there are difficulties like shoulder dystocia that are not managed properly, potentially leading to common birth injuries.
- Failure to Monitor Fetal Distress: Inadequate monitoring of fetal heart rate by nursing staff or a physician’s failure to recognize and promptly respond to signs of distress. This can lead to Nursing Negligence Birth Injury or Physician Negligence Birth Injury.
- Delayed C-Section: Failure to perform a timely Cesarean section when the baby is in distress.
These preventable medical errors often form the basis of birth injury claims and birth injury lawsuits, especially Hypoxic-Ischemic Encephalopathy Claims.
Impact and Legal Implications of Anoxic Hypoxic Brain Injury
The long-term impact of Anoxic Hypoxic Brain Injury can range from mild cognitive impairments to severe cerebral palsy, developmental delays, and lifelong reliance on Adaptive Equipment Birth Injuries necessitate. The extensive lifelong care often requires substantial birth injury compensation.
When pursuing a legal claim, expert witnesses play a crucial role. Expert Witnesses Birth Injury Lawsuits demand, including neurologists and neonatologists, can explain the specific type of Anoxic Hypoxic Brain Injury, its cause, and the resulting damage, using Medical Records Birth Injury Claim elements as evidence.
If your child suffered an Anoxic Hypoxic Brain Injury and you suspect medical negligence, a birth injury lawyer can help you understand the nuances of your case and pursue the justice and compensation needed for your child’s future.
If you want to call us and book a free call to discuss Anoxic Hypoxic Brain Injury and your legal options, contact here: Contact Trusted Birth Injury Lawyers | CPFamilyHelp
Frequently Asked Questions (FAQ) about Anoxic Hypoxic Brain Injury
Is HIE considered an Anoxic Hypoxic Brain Injury?
Yes, HIE (Hypoxic-Ischemic Encephalopathy Claims) is a form of hypoxic-ischemic brain injury, meaning it involves both reduced oxygen (hypoxia) and reduced blood flow (ischemia). It is a significant category within Anoxic Hypoxic Brain Injury
What are the immediate signs of Anoxic Hypoxic Brain Injury in a newborn?
Immediate signs can include low Apgar scores, seizures, difficulty breathing, poor muscle tone (floppiness), and abnormal reflexes. These symptoms can alert medical staff to potential Anoxic Hypoxic Brain Injury.
Can Anoxic Hypoxic Brain Injury be prevented?
Many cases of Anoxic Hypoxic Brain Injury are preventable if medical professionals properly monitor the mother and baby during labor, recognize signs of distress, and intervene promptly and appropriately (e.g., through a timely C-section). This relates to Hospital Protocols Birth Injury Prevention.
How does the type of Anoxic Hypoxic Brain Injury impact a legal claim?
The specific type and severity of Anoxic Hypoxic Brain Injury (anoxic vs. hypoxic, and the extent of damage) directly impact the child’s prognosis and lifelong needs, which in turn determines the birth injury claim value and the strategies for Life Care Planning Birth Injury.
What kind of Long-Term Therapies Birth Injuries need for oxygen deprivation?
Children with Anoxic Hypoxic Brain Injury often require intensive Long-Term Therapies Birth Injuries necessitate, including physical therapy, occupational therapy, speech therapy, and possibly cognitive rehabilitation, to maximize their development.





Traumatic Brain Injury Birth Lawyer: 5 TBI & Cerebral Palsy Claims
[…] challenges related to movement, cognition, and overall development. If your child sustained a traumatic brain injury during birth that you believe resulted from medical negligence, the emotional devastation and […]